Course Content
-
Pediatric Heart Failure: “How to approach the management of Pediatric Heart Failure” Understanding heart failure: the basics in pediatric heart failure and congenital heart diseases. Basics of treatment and decision making in clinic cases
- Introduction. Definition of Heart Failure
- Etiology of Heart Failure in pediatric age
- Pathophysiology of Heart Failure
- Heart Failure in Congenital Heart Disease
- Natriuretic peptid system
- Biomarkers in Heart Failure
- Signs and Symptoms in pediatric age
- Classification of severity in pediatric Heart Failure
- Different forms of cardiomyopathies: “Diagnostic techniques and treatments”
- Dilated Cardiomyopathy
- Myocarditis
- Hypertrophic Cardiomyopathy
- Restrictive Cardiomyopathy
- Non-compaction Cardiomyopathy
- Arrhythmogenic Right Ventricular Dysplasia (ARVD)
- Evaluation Cardiomyopathies and Genetics
- Evaluation Quiz
- Arrhythmias in Pediatric Heart Failure: EKG abnormalities
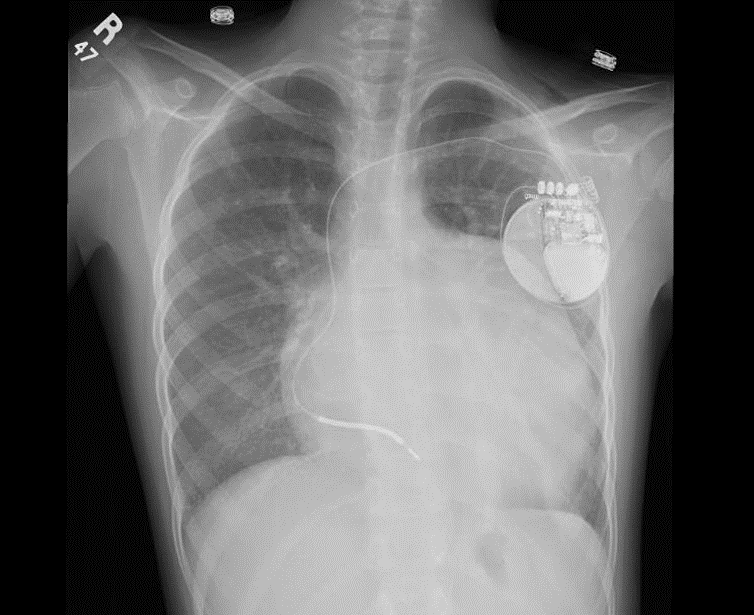
- Indications ICD in adults and pediatric age
- Clinic Cases. Quiz
- Treatment in chronic pediatric Heart Failure
- New treatment: Sacubitril – Valsartan
- New therapies and Experimental
- Summary Pediatric Heart Failure therapies
-
Basic and Advanced Echocardiography in Pediatric Heart Failure Description of basic and advanced echocardiography tools for diagnostic and follow-up of children affected by heart failure
- Journal Club: “Basic and advanced echocardiography in advanced heart failure: an overview”
- LV systolic function
- RV systolic function
- Cardiac Diastolic Function and Diastolic Heart Failure
- Tissue Doppler Imaging (DTI) and diastolic dysfunction
- Summary Echo left diastolic dysfunction
- RV diastolic dysfunction
- Management of pediatric diastolic dysfunction
- Clinic Cases
- dP/dt LV function assessment
- Myocardial Performance Index (Tei Index) Doppler Mitral Flow
- Myocardial Performance Index (Tei Index) DTI
- Basics of Strain and Strain-rate
- Global longitudinal Strain (GLS)
- Cardiac output assessment by Echo
- Advanced Imaging in Pediatric Heart Failure
- Echocardiography: Apps and webs
- Clinic Cases
-
Pediatric Heart Transplant (I) Basic in inmunology and rejection. Indications of pediatric heart transplant and contraindications. Mechanical support in pediatric age. Surgery and perioperative treatment.
- Basis of transplant immunology
- Human leucocytes antigen (HLA)
- Blood group antigen (ABO)
- Graft Rejection
- Donor selection & evaluation
- Tissue typing and cross matching
- Ischemic time and the TransMedics® Organ Care System (OCS™)
- Indications and Contraindications of Pediatric Heart Transplant
- Indications of pediatric Mechanical cardiac support (MCS)
- Types of Devices for pediatric MCS
- VAD selection for pediatric MCS
- Surgery of Heart Transplant in pediatric age and in Congenital heart disease
- Principle Challenge in immunosuppressive therapies
- Induction therapy during surgery, postoperative period and denervated heart
-
Pediatric Heart Transplant (II) Basic of immunosuppression treatment. Management of rejection and infections in pediatric heart transplant. Information for patients and relatives. Outcomes of heart transplant and indications of retransplantation
- Basis of immunosuppression therapy
- Risk of infection after transplantation
- Complication of chronic immunosuppression
- Basis of Rejection and assessment
- Endomyocardial biopsy and rejection
- Treatment of humoral and cellular rejection
- Chronic rejection: Coronary Artery Vasculopathy (CAV)
- Clinic follow-up in patient transplanted
- Cardiac Rehabilitation in pediatric heart transplant
- Survival and Causes of death in pediatric heart transplant
- Indications of retransplantation and survival
- Home Care after Pediatric Heart Transplant
- Palliative care in Pediatric Heart Failure and Heart Transplantation
- Future perspectives. Summary
- Clinic cases
-
Final Quizz Congratulations! You finished the course, check your knowledge with this final test
-
Fellow Evaluation Course Evaluation of the cardiac fellows who attended the course in May 2020
Indications ICD in adults and pediatric age
The population of children and young adults requiring a cardiac pacing device has been consistently increasing. The knowledge of indications, pacing leads and devices, anatomical variations and the technical skills required are different than that required in the adult population
Who should consider an ICD ?
The main indications for use of an ICD can be divided into 2 groups:
- Secondary prevention of sudden cardiac death (SCD) in patients with prior sustained VT, VF or resuscitated SCD thought to be due to VT/ VF
- Primary prevention of SCD in patients at increased risk of life-threating VT/ VF
The reasons for using ICD have expanded in adults and children population, including in chronic heart failure.
Who should consider an ICD ?
Sudden cardiac death (SCD) in childhood and adolescence is associated with congenital heart disease, cardiomyopathies, and genetic arrhythmia syndromes
ICDs are recommended for patients who have survived an episode of cardiac arrest, patients with poor cardiac function with evidence of moderate to severe heart failure, patients with inducible ventricular dysrhythmia in a setting of symptomatic CHD and in patients with genetic cardiomyopathy.
ICDs may also be considered as a bridge to orthotopic heart transplantation in pediatric patients, particularly given the longer times to donor procurement in younger patients.
There is paucity of clinical experience and data regarding ICD implantation for primary prevention of SCD in young patients and therefore recommendations are based on extrapolation of data from adult studies. In adults indication of ICD Class I is in case of LVEF< 35% and NYHA 2 or 3, in children we have to balance de risk of the procedure and benefits, and currently as second prevention is just worlwide accepted. Miniturization of ICD devices and ICD subcutaneous will change surely the indications in next years.
References:
1.Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2018; 72:e91.
2.Ganz L et al. Implantable cardioverter-defibrillator: Overview of indications, components and functions, 2018. En: Lee S, ed Waltham Mass. Up to Date.
3.Asakai H, Shimizu A, Mitsuhashi T, Ueyama T, Yokoshiki H, Nishii N et al. Current Trends in Implantable Cardioverter-Defibrillator Therapy in Children: Results From the JCDTR Database. Circ J. 2018 Oct 20. doi: 10.1253/circj.CJ-18-0712.
4.Russo AM, Stainback RF, Bailey SR, et al. ACCF/HRS/AHA/ASE/HFSA/SCAI/SCCT/SCMR 2013 appropriate use criteria for implantable cardioverter-defibrillators and cardiac resynchronization therapy: a report of the American College of Cardiology Foundation appropriate use criteria task force, Heart Rhythm Society, American Heart Association, American Society of Echocardiography, Heart Failure Society of America, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol 2013; 61:1318.
5.Singh HR1, Batra AS, Balaji S. Cardiac pacing and defibrillation in children and young adults. Indian Pacing Electrophysiol J. 2013;13:4-13.


