I am pregnant and my baby has an abnormal heart detected by fetal echocadiography, what should I do?
Cardiac abnormalities can be diagnosed during pregnancy. The heart of the fetus starts to develop during the first weeks of gestation. Having a cardiac malformation can be associated with malformations of other organs or genetic abnormalities, which is the reason of amniocentesis or chorial biopsy are performed, to rule out gene alterations.
The obstetrician during pregnancy performs ultrasounds to see the development of the organs and the growth of the fetus. Keep in mind that ultrasounds are performed through the mother’s abdominal wall and all the cardiac structures of the fetus are not always visible, in addition the fetal circulation is different from the neonatal circulation.
During pregnancy, it is important to monitor the adequate growth of the fetal cardiac chambers, with no predominance of any of them. When a wider chamber is detected compared to the other, it may indicate that there is some problem in the the heart. In addition, the obstetrician has to observe that the vessels intersect (the pulmonary and aortic arteries intersect in the normal heart, if they are parallels could mean an abnormality).
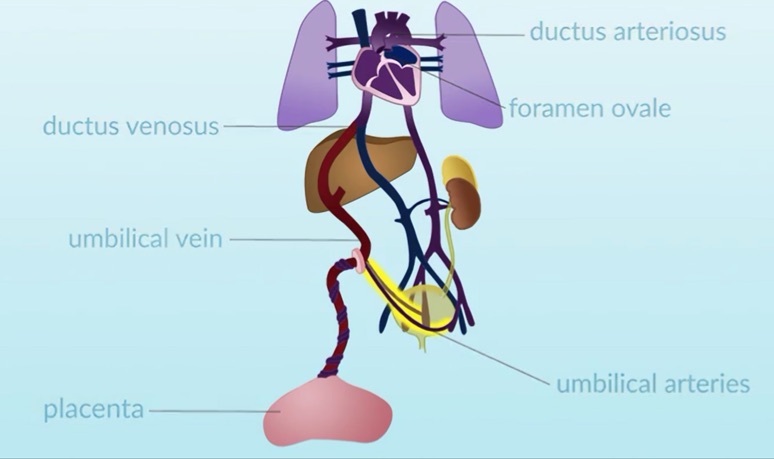 Fetal circulation (adapted from https://www.openpediatrics.org/assets/video/fetal-circulation)
Fetal circulation (adapted from https://www.openpediatrics.org/assets/video/fetal-circulation)
If both vessels (aortic and pulmonary) are in “parallel” means that they are arising from different ventricle, this anomaly is called: Transposition of great arteries, and a cardiac surgery will be needed during neonatal period.
If your obstetrician is not sure regarding the echo findings, or the fetal heart is not seen appropiately, a specific fetal echocardiography has to be performed.
Normally the best time to see the heart is at 20 weeks of gestation, although there is currently the possibility of performing an early echocardiography (between week 14-16 of gestation). This echocardiography should be carried out by experts, obstetricians experienced in fetal echocardiography, or pediatric cardiologists.
Is there any treatment which can improve the fetal heart?
Some abnormalities worsen throughout the pregnancy and some interventions could be carried out during pregnancy (called “fetal interventionism”). A dilation of the aortic or pulmonary valve can be performed (valvuloplasty). Across a puncture a catheter with a balloon is inserted through the abdominal wall’s mother and the thorax of the fetus, and through the cardiac ventricle the balloon is positioned in the narrow area and can be dilated. With this valvuloplasty, the corresponding ventricle, left (if it is an aortic valvuloplasty) or right (if it is a pulmonary valvuloplasty), can be prevented from developing properly.
In addition, the foramen ovale (hole in the upper part of the fetal heart, which redirects the more oxygenated blood from the placenta to the baby’s brain) can be dilated when needed. With the exception of these cases, the vast majority of cardiac malformations are untreated during pregnancy.
Please send an email to niakoroweb@gmail.com, if you require more information



